Management of Urethral Stricture Disease
When a scar following injury or infection blocks or slows the flow of urine, it is called a urethral stricture. In addition to uncomfortable urinary symptoms such as reduced flow rate and more frequent urination, a urethral stricture can lead to complications that include urinary tract infections, prostatitis, urinary retention and kidney damage.
}})
In cases of emergency, like sudden blockage of urine, to divert the urine stream, the doctor may initially put a catheter directly into the bladder (trocar cystostomy) by making a small incision in the lower abdomen. This may also be required in other conditions like the presence of renal failure due to stricture, urinary tract infection or periurethral abscess, fistula etc.
In all other situations, for specific therapy, the doctor after studying the length, location and cause of the stricture will plan further treatment. The treatment options are:
VIU (Visual Internal Urethrotomy) is an endoscopic procedure. In this procedure, an endoscope is passed into the urethra, the area of narrowing visualized and incised with an endoscopic knife. A catheter is kept for 3 days post-procedure. This is acceptable when the stricture in the urethra is less than 1 cm long and the operation is done for the first time. Recurrence is common if it is done for longer strictures or very dense strictures. The doctor may advise regular self-dilatation by passing an appropriately sized catheter.
Open surgical urethral reconstruction
Many different reconstructive procedures have been used to treat strictures. In all cases, the choice of repair is influenced by the characteristics of the stricture and no single repair is appropriate for all situations. Open reconstruction of a short urethral stricture may involve surgery to remove the stricture and reconnect the two ends (anastomotic urethroplasty). When the stricture is longer than 2-3 cm, repair by tissue transfer is required to enlarge the segment to normal (substitution procedures). Substitution repairs may need to be performed in stages in difficult circumstances.
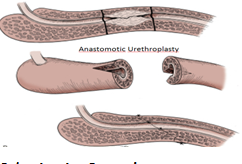
Anastomotic Procedures
These are usually reserved for less than 2cm urethral strictures where the urethra can be joined after removing the stricture. This procedure involves an incision between the scrotum and anal opening. A urethral catheter will be left for 14 days and removed.
Substitution Procedures
Buccal Mucosal Graft Urethroplasty: Longer strictures will be repaired with a free graft to enlarge the urethra. The graft is harvested from inside the cheek and the length of graft required will depend on stricture length. The graft may be taken from one or both cheeks and/or the under surface of the tongue. This is usually performed as an inpatient procedure with 3-4 days of hospitalization. The urethral catheter will be removed after three weeks.

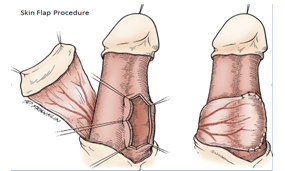
Skin Flap Procedure
When there is a long stricture in penile urethra, the cause being non-BXO (Balanitis Xerotica Obliterans), associated with severe scarring and a free graft would not survive, flaps of penile skin can be rotated to patch the urethra. The catheter will be removed after 2-3 weeks.
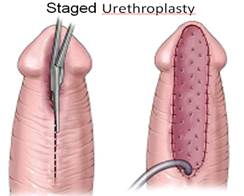
Staged Procedure: When sufficient local tissue is not available for a skin flap procedure and local tissue factors are not suitable for a free graft, a staged procedure may be required. The first stage in a staged procedure focuses on opening the underside of the urethra to expose the complete length of the stricture. A graft is secured to the edges of the opened urethra and allowed to heal and mature over a period of three to six months. During that time, patients urinate through a new opening behind the stricture, which in some cases will require the patient to sit down to urinate. The second stage is performed after the graft around the urethra has healed and is soft and flexible. At this stage the graft is formed into a tube and the urethra is returned to normal. A catheter will be left for 10 to 21 days.
All patients who undergo any of the above procedures, require a follow up at regular intervals to look for any recurrence of narrowing. The success rate after the anastomotic procedure is about 90-95% whereas buccal graft is 85-90%. Those patients who have a BXO, the success rate is around 70-80% over a 5 year period. After surgery, if recurrence is detected, either an endoscopic procedure or sometimes a repeat surgery may be needed.
Urinary symptoms may worsen over a period of time. It may also cause frequent urinary tract infection, testicular infections, acute urine block or kidney damage due to back pressure changes and infections.
It is usually not contagious but the underlying cause, like an STD, may be contagious.
Avoid injury to the urethra and pelvis. In patients on self-catheterization, use a smaller size catheter after adequately lubricating the urethra. Those caused by sexual contact can be prevented by using condoms.